July 2025 broke down the door. Just days after the Supreme Court gave the Trump administration the green light on July 8 to push forward with government wide job cuts, Health and Human Services dropped a bombshell. Thousands of federal employees were told they’d be out as of July 14.
The plan was to cut around 10,000 jobs, slashing the department’s workforce from roughly 82,000 down to 62,000. Officials are touting a savings of 1.8 billion dollars each year, but the backlash has been swift. Public health leaders and unions are already sounding alarms, warning that this is not just trimming fat, it is cutting into muscle and bone.
Background

This didn’t happen overnight. The Trump administration has been angling for years to slim down the federal health system, arguing that agencies like HHS had become bloated and inefficient.
The groundwork was laid early in 2024 with hiring freezes and voluntary buyouts meant to nudge staff out the door. Now, that long buildup has exploded into mass layoffs that hit not just HHS but also the CDC, the NIH, and the FDA. And here is the hard truth: these are not just job titles being erased. Each of these positions carries decades of specialized knowledge that cannot simply be replaced by a new hire fresh out of graduate school.
Agencies and Programs Most Impacted

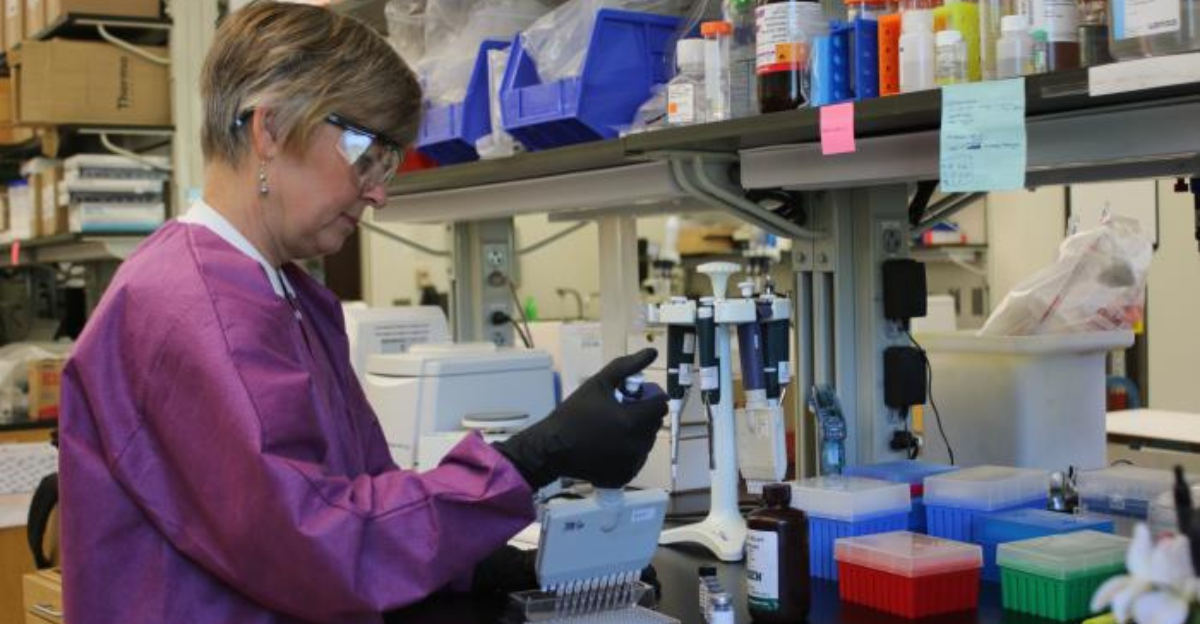
The CDC is getting hammered the hardest. Teams that once monitored HIV outbreaks, reproductive health data, and workplace safety standards are now running at half strength. Some divisions are so short staffed they look like ghost towns. At the NIH, researchers who dedicated years to developing lifesaving drugs are clearing out their offices. And the FDA has been running on fumes for years, and now it has lost another wave of inspectors and technical experts who keep an eye on food safety and tobacco regulation.
Even the behind-the-scenes staff (people who handle logistics, contracts, and communication) have been gutted. The result is a system that is moving slower and one major crisis away from stalling completely.
The Catalyst

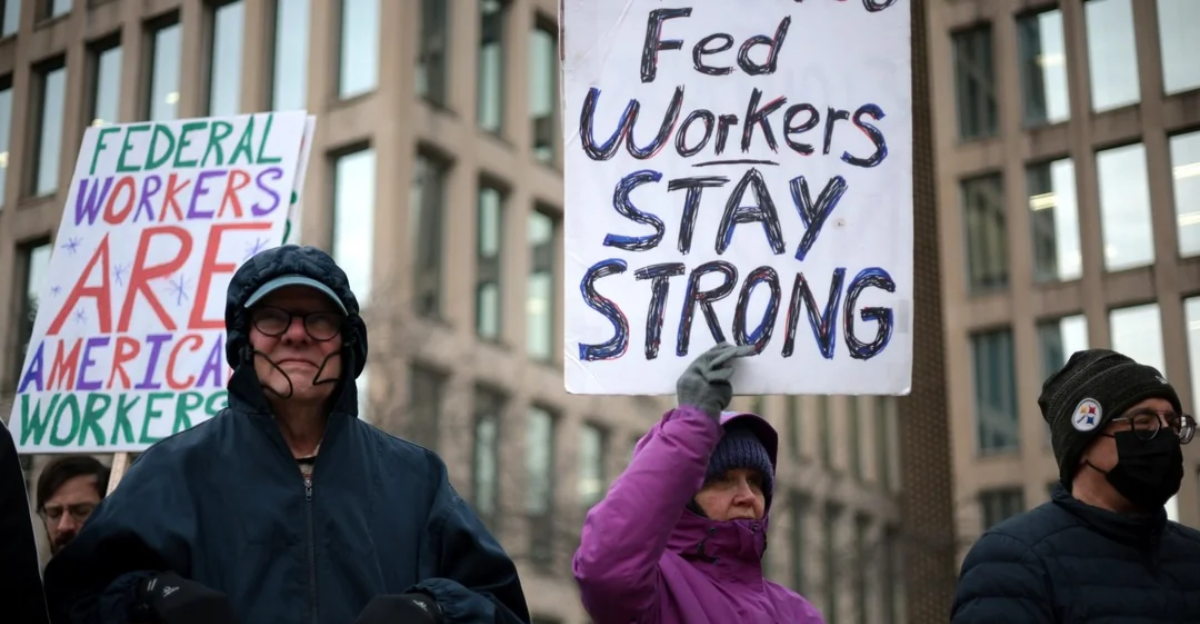
The turning point came when the Supreme Court removed the freeze on these workforce reductions in early July. Overnight, thousands of workers were told their jobs were gone. Some employees found out via email while others were met with silent, locked offices. Lawsuits are already flying in from states and unions, accusing the administration of gambling with public health. For many workers, the court’s decision landed like a punch to the gut after months of limbo and quiet dread. Now the health system is staring down the next flu season or surprise outbreak with fewer hands, fewer resources, and a level of vulnerability it hasn’t faced in decades.
Emergency Warnings and Sector Response

The warnings are getting louder by the day. Former CDC directors and groups like the American Public Health Association are calling this a dangerous gamble. They say epidemic preparedness, which already took a hit during the pandemic years, could collapse without enough trained professionals to staff key programs.
State and local health departments are already seeing cracks appear. Funding and guidance for STI testing, smoking cessation programs, and outbreak tracking are drying up. Some experts have even suggested that a routine flu season could turn deadly if federal support falters. Their message is blunt: this is not a bureaucratic shakeup. This is a direct hit to the country’s ability to protect its people.
Intended Rationale vs. Expert Concerns
HHS officials continue to repeat that these layoffs are about efficiency and cost control. They claim that the cuts will save around 1.8 billion dollars annually and allow the department to refocus on what they call its core priorities, like chronic disease prevention.
Critics, including many former agency leaders, argue that this logic is painfully short sighted. Vaccine research, disease tracking, and emergency response are not optional luxuries. They are foundational. And while cost savings sound good in a press release, they mean little when the country is left scrambling during the next public health emergency. The question is no longer about efficiency. It is about survival.
Real World Effects

The impact of these cuts is already rippling out. Outbreak investigations are slower. Family planning and maternal health programs are losing crucial federal support. Immunization drives that once moved like clockwork are now lagging for weeks at a time. NIH research projects have been paused midstream. FDA inspections are stacking up like forgotten homework. Every number on a layoff list represents years of expertise, often from people who were the backbone of these programs. You cannot replace that with a quick hire or a software tool. When the next health scare arrives, the question is not whether cracks will show; it is how deep and how wide they will run.
Legal and Ethical Controversies

The lawsuits are piling up. States are accusing the administration of violating federal obligations and risking lives for political points. Critics also highlight how transparency is eroding. Many of the employees who were laid off were responsible for public data reporting and communication. Now reporters say they are hitting walls where there used to be open channels. What began as a fiscal debate has morphed into a national argument about ethics, accountability, and whether gutting these agencies was ever a fight worth having.
The Broader Context

The timing feels like a bad joke. The World Health Organization is sounding the alarm about funding gaps and international health risks. Meanwhile, the United States is struggling with some of the worst maternal health outcomes among wealthy nations.
Diseases we thought we buried, like measles and tuberculosis, are creeping back. Add a surge in mental health crises and rising drug overdose deaths, and you get a public health system already straining under the weight. Now, with 10,000 fewer federal workers, even small problems could spiral into disasters.
And in a world where disease spreads faster than news headlines, that is a terrifying prospect.
Conclusion

The layoffs at HHS may be seen as smart budgeting by the administration, but in actuality, it is more like a roll of the dice with America’s safety net. Supporters keep tossing around words like efficiency and streamlined operations, but on the ground, the system looks like it is being held together with duct tape and desperation. The lawsuits might drag on for months or years, yet the damage is already baked in. The expertise and institutional memory that once held this system steady are gone.
The question now is simple and brutal: will this be remembered as reform, or as one of the biggest public health blunders in modern history? Well, that depends on how well states and local agencies can patch the gaps. Right now, the future of federal health readiness feels like a fragile gamble, and everyone is watching to see what breaks first.
